Grand Canyon University Nursing Change Project Evaluation Plan
Grand Canyon University Nursing Change Project Evaluation Plan
Review your strategic plan to implement the change proposal, the objectives, the outcomes, and listed resources. Develop a process to evaluate the intervention if it were implemented. Write a 150-250 word summary of the evaluation plan that will be used to evaluate your intervention.
The assignment will be used to develop a written implementation plan.
ORDER NOW FOR CUSTOMIZED SOLUTION PAPERS
Objectives for the proposed Interventions Example
The proposed capstone intervention aims at surgery nurses through the development of relaxation measures to avoid burnout among nurses. The objectives of the interventions include; first, to ensure nurses become fully immersed in the present and forgo past regrets and worries about the future (Asuero et al., 2014). By taking into consideration, surgery is among the most complex exercise undertaken in the healthcare sector, mindfulness will improve relaxation and techniques of handling unpleasant situations or emotions. Therefore the nurses will have a significant reduction in exhaustion and increase individual accomplishments, which will reflect on the quality of services they render.
Second, to ensure graduate nurses have a smooth transition. The intervention will help freshman nurses to fell prepared, so they can handle the workload and stress that comes with the surgery nurse profession; therefore, not place the freshman health workers in a vulnerable situation that can evoke immense emotions of frustration. The program will enable effective cross-team connectivity among surgery nurses and nursing students, which will promote a supportive environment( Rudman & Gustavsson, 2011).
Lastly, to encourage self-care among the surgery nurses. Although it may be challenging to achieve, especially since some nurses are workaholics and rarely take breaks. However, when the health center provides a section in which nurses can visit and participate in the communicative exercise, they will be able to relive the mind and can resume work less exhausted.
References
Asuero, A. M., Queralto, J. M., Pujol-Ribera, E., Berenguera, A., Rodriguez-Blanco, T., & Epstein, R. M. (2014). Effectiveness of a mindfulness education program in primary health care professionals: A pragmatic controlled trial. Journal of Continuing Education in the Health Professions, 34(1), 4-12.
Rudman, A., & Gustavsson, J. P. (2011). Early-career burnout among new graduate nurses: A prospective observational study of intra-individual change trajectories. International Journal of Nursing Studies, 48, 292-306. doi: 10.1016/j.ijnurstu.2010.07.012
Example Resource Evaluation
Inadequate physical resources, overtime, unbalanced nurse-patient proportions, stressful practice environments, tight timelines, and imbalanced workloads negatively influence nurses’ perceptual experience of the caliber of the nursing profession surrounding. As perceived by nurses and patients, the nursing environment makes for a critical responsibility in contracting and keeping back experienced and skilled human resources. Various resourcefulness is needed to implement the proposal for nurse burnout interventions.
- Financial resources: -adequate finances will be needed to equip under-equipped healthcare providers. Additionally, funds will be required in recruitment drives for qualified and sustaining improved wages for competent nurses. Ultimately, financial resources are needed to set up better communication strategies and maintain established surgery centers to minimize burnout levels.
- Sufficient and appropriate equipment: – we acknowledge the crucial responsibility of tangible material, for example, ultramodern workplace equipment, for instance, enablers of surgical and care activities. According to a professional view, faulty equipment is a significant barrier in surgical rooms, leading to misappropriated handling, disruption, emotional tensions, and delay in delivery of care.
- Well qualified nurses: -staffing is a broad term. It not only pertains to a reliable count of nurses but having adequately trained nurses relating to technical skills and theoretical cognition. Qualified staff can utilize decisive reasoning and therefore make proper and timely objective determinations. Also, staffing, along with expertise, leads to the appropriate utilization of available resources, thereby reducing overall burnout.
- Necessary physical infrastructures: -sufficient physical space and an adequate spacing within the wards and theatres. An imbalanced workload due to congestion is crucial in determining burnout, anticipating flip over, and discontentment amongst nurses.
Generally, physical resources and adequate staff are the main highlighted elements within surgery nurses practicing the profession that significantly influence nurses’ perceptual experience (Wentzel & Brysiewicz, 2017). If these resources are availed, the proposed interventions on nurse burnout are likely to prove beneficial.
References
Wentzel, D, & Brysiewicz, P. (2017). Integrative review of facility interventions to manage compassion fatigue in oncology nurses. Oncol Nurs Forum. 44(3).
Capstone Change Project Evaluation Plan
The assignment will be used to develop a written implementation plan.
Step 1) Review your strategic plan to implement the change proposal, the objectives, the outcomes, and listed resources.
Step 2) Develop a process to evaluate the intervention if it were implemented.
Step 3) Write a 150-250 word summary of the evaluation plan that will be used to evaluate your intervention.
Address the following in your summary:
What data was collected?
What tool will be used to collect the data?
Who will be responsible for collecting data?
How will this data be communicated to the team?
Capstone Change Project Evaluation Plan Example
An evaluation plan is essential in monitoring the effectiveness of evidence-based practice (EBP) after implementation. It involves data collection and compares the post-intervention with the pre-intervention outcomes. A positive outcome would be an improvement in the primary outcomes. Therefore, if this project were to be implemented, an evaluation plan would be necessary to assess the level of nurses’ knowledge as well as the incidence of ventilatory-associated pneumonia (VAP). Data collection would include the use of surveys and interviews. The survey will include a clinical pulmonary intervention (CPI) scale that assesses various parameters of VAP. Conversely, interviews would be essential in assessing nurses’ knowledge and experience with the intervention. Structured questionnaires with both open-ended and closed-ended questions will be relevant to be used. Such will help in making adjustments and improving the approach to the EBP. Besides, both qualitative and quantitative data will be collected.
During data collection, I would prefer to be involved. However, I would welcome the assistance of my preceptor to help me identify focused members who can collect quality data. I will also involve nurse leaders during data collection. The collected data will provide a comparison to assess the effectiveness and make a decision. Performance of the outcomes below the expected level will require re-evaluating the implementation plan to make adjustments that suit the project change. Finally, I will communicate the results to my team members while allowing for contributions. The collected information can be printed for members to review or use in a presentation. The data can be addressed either through online channels such as webinars and social media, conference halls, or during stakeholder meetings. Such arrangements ensure that all data can be reviewed and then verified.
Professional Capstone and Practicum Reflective Journal
Students are required to submit weekly journal entries throughout the course. These reflective narratives help students identify important learning events that happen throughout the course and the practicum. In each week\’s entry, students should reflect on the personal knowledge and skills gained.
Write a reflection journal (250-300 words) to outline what has been discovered about your professional practice, personal strengths and weaknesses, and additional resources that could be introduced in a given situation to influence optimal outcomes. Each week there will be a specific focus to use in your reflection. Integrate leadership and inquiry into the current practice. Please make sure to address all areas in your writing.
Topic Focus: The Role of Technology in Improving Health Care Outcomes
While APA style is not required for the body of this assignment, solid academic writing is expected.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
You are required to submit this assignment to LopesWrite. A link to the LopesWrite technical support articles is located in Class Resources if you need assistance.
Professional Capstone and Practicum Reflective Journal Sample
This week, I spent some time with my preceptor to discuss the role of technology in improving healthcare outcomes. I realized that technological development positively impacts patient care and health outcomes through revolutionization. This is because technology can be used in every step of patient care, including triaging, diagnosis, management, and follow-up of patients. Besides, technology offers an opportunity for transforming and improving healthcare in terms of reducing errors, improving care coordination, tracking records, and improving practice efficiency (Tummers et al., 2020). For instance, telemedicine is an example of technology currently being used to manage patients with chronic conditions such as diabetes mellitus.
Using telemedicine, the healthcare provider and the patient are connected and easily communicate to enhance care. Patients can self-monitor blood sugars in remote areas while the caregiver is aware of the readings. In case of any abnormal findings, an intervention is provided quickly. Furthermore, telemedicine improves check-ups and scheduling and reduces the need for paperwork. As a result, patient sugars are well controlled, resulting in improved health outcomes and a reduction in mortality, morbidity, and other complications associated with diabetes.
Another aspect of technology is the use of information management systems, which have improved efficiency and speed in the services provided. Furthermore, it improves communication between different departments, a factor that ensures care is coordinated through enhanced information sharing (Tummers et al., 2020). Doctors and other healthcare providers can also share information worldwide through improved communication to enhance care. Finally, technology allows nurses to search for information in evidence-based practice that helps guide care during decision-making. Therefore, it is prudent that all healthcare settings acquire various technologies to improve health outcomes.
Reference
Tummers, M., Kværner, K., Sampietro-Colom, L., Siebert, M., Krahn, M., Melien, Ø., Hamerlijnck, D., Abrishami, P., & Grutters, J. (2020). On the integration of early health technology assessment in the innovation process: reflections from five stakeholders. International Journal of Technology Assessment in Health Care, 36(5), 481–485. https://doi.org/10.1017/S0266462320000756
Benchmark – Capstone Project Change Proposal SUBMIT ASSIGNMENT
In this assignment, students will pull together the capstone project change proposal components they have been working on throughout the course to create a proposal inclusive of sections for each content focus area in the course. For this project, the student will apply evidence-based research steps and processes required as the foundation to address a clinically oriented problem or issue in future practice.
Develop a 2,500-4,000 written project that includes the following information as it applies to the problem, issue, suggestion, initiative, or educational need profiled in the capstone change proposal:
Background
Clinical problem statement.
Purpose of the change proposal in relation to providing patient care in the changing health care system.
PICOT question.
Literature search strategy employed.
Evaluation of the literature.
Applicable change or nursing theory utilized.
Proposed implementation plan with outcome measures.
Discussion of how evidence-based practice was used in creating the intervention plan.
Plan for evaluating the proposed nursing intervention.
Identification of potential barriers to plan implementation, and a discussion of how these could be overcome.
Appendix section, for evaluation tools and educational materials, etc. are created.
Review the feedback from your instructor on the PICOT Question Paper, and Literature Review. Use this feedback to make appropriate revisions to these before submitting.
Prepare this assignment according to the guidelines found in the APA Style Guide, located in the Student Success Center.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
You are required to submit this assignment to LopesWrite. A link to the LopesWrite technical support articles is located in Class Resources if you need assistance.
Benchmark Information
This benchmark assignment assesses the following programmatic competencies:
RN to BSN
1.4: Implement patient care decisions based on evidence-based practice.
2.2: Manage patient care within the changing environment of the health care system.
Benchmark- Capstone Project Change Proposal Example
Background
Admission of patients into the intensive care unit (ICU) is a common health practice worldwide. In the US alone, over 5 million people were admitted to the ICU (Suljevic et al., 2020). Patients in the ICU are provided with specialized care that requires close monitoring of medications and equipment. Because most of the patients are unconscious due to either sedating medications or severe disease, they require close monitoring to stabilize all body systems to improve outcomes. As a result, ICU patients require life-saving invasive procedures aimed at stabilization. Among the common procedures include central lines, urinary catheters, endotracheal intubation, tracheostomy, feeding tubes, and cardiac monitors (Suljevic et al., 2020). Ironically, despite these procedures being paramount in saving lives, they contribute to infections and other complications that are major contributors to death. For instance, catheters are associated with catheter-associated urinary tract infections (CAUTIs); central lines cause central line-associated bloodstream infection, while mechanical ventilators are associated with mechanical ventilators (VAP).
The presence of VAP or either of the infections in ICU patients complicates their clinical outcomes while increasing the risk of mortality and morbidity and increasing the cost of care. Therefore, preventing the incidence of such infections remains a priority issue in health care. Some of the nurse-led evidence-based practice preventive measures include encouraging early ambulation, hourly turning, installation of orotracheal as opposed to nasotracheal tubes, spontaneous breathing trials, sedation, head elevation, staff education, infection surveillance, and prophylaxis for stress ulcers and venous thromboembolism (Xu et al., 2019). These methods have helped in reducing the incidents of VAP but are not sufficient. The need to improve patient outcomes has led to various pieces of research using chlorohexidine (CHG) mouthwash to evaluate its effectiveness in preventing VAP while improving patient outcomes. There have been mixed findings from evidence. Most studies have proposed using CHG to prevent VAP and other infections, while some show contradictory results. Therefore, in my quest to understand the subject matter, I decided to undertake this project to find more evidence that will help in improving patient outcomes. This paper will address the following: problem statement, PICOT statement, the purpose of the change proposal, literature search strategy, literature evaluation, and barriers to implementation, as well as how to overcome them.
Clinical Problem Statement
By definition, VAP is a lower respiratory tract disorder that develops within 48 hours or more of being on mechanical ventilation in a patient who originally did not have the condition. VAP is among the most common nosocomial infections in ICU, accounting for 9 to 27% of all infections in the ICU. It is the second commonest hospital-acquired infection (HAI) after CAUTIs (Xu et al., 2019). Because up to 300,000 patients admitted to the ICU require mechanical ventilation to support breathing and necessitate gaseous exchange, up to 20% of all VAP associated with mechanical ventilators is the major risk factor (Suljevic et al., 2020). The ventilators act as a breach in the natural immunity that allows bacteria and other micro-organisms to access the lower respiratory tract and multiply to cause VAP. In addition, intubation compromises the integrity of the trachea and oropharynx, allowing oral and gastric secretions to access the respiratory tract, leading to irritation that further increases the risk of VAP. The incidences of VAP increase with the duration of ventilation, with an estimated rate of 3% in the first days, 2% per day between days 6 and 10, and 1% per day after day 10 (Suljevic et al., 2020). Notably, an infection caused by Pseudomonas contributes to crude mortality of 27 to 67% with VAP, which is higher than all other bacteria except for actinobacteria (Xu et al., 2019). In addition to mechanical ventilation, other risk factors combine to increase the risk, such as advanced age, immobilization, supine position, immunosuppression, and increased ICU stay.
Various microorganisms are implicated in the pathophysiology of VAP. Both gram-positive and gram-negative bacteria can colonize the lower respiratory tract, multiply, and cause pneumonia (Kohbodi et al., 2022). Comparing the timing of infection, early-onset VAP is associated with drug-sensitive bacteria, while late-onset VAP is associated with drug-resistant bacteria. Drug resistance pneumonia is difficult to treat and impairs patient outcomes. Furthermore, VAP increases the risk of mortality and morbidity for those who survive and increases hospital stay. For instance, every patient spends an extra $40,000 on each extra day spent in the hospital, leading to an increased healthcare burden (Pawlik et al., 2022). Therefore, there is a need to prevent VAP and increase patient outcomes.
The purpose for Change.
Because of the burden caused by VAP in terms of increased hospital stay, mortality, morbidity, and increased cost of care, there is a need to implement a nurse-driven protocol to prevent infection. Among the various protocols used in the prevention, chlorohexidine (CHG) has been applied in various setups, yielding promising results. CHG is an antiseptic antimicrobial with a bactericidal effect against both gram-positive and gram-negative bacteria. Appropriate use of CHG mouthwash reduces the microbial load and helps in reducing the incidences of VAP, as reported by various pieces of evidence (Kohbodi et al., 2022). Therefore, this project change aims to improve nursing knowledge about the use of CHG in preventing infections in the ICU. This will help reduce the rate of nosocomial infections while improving patient outcomes and reducing mortality, hospital stay, and cost of care.
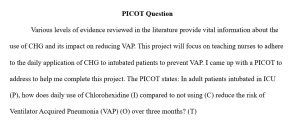
PICOT Question
Various levels of evidence reviewed in the literature provide vital information about the use of CHG and its impact on reducing VAP. This project will focus on teaching nurses to adhere to the daily application of CHG to intubated patients to prevent VAP. I came up with a PICOT to address to help me complete this project. The PICOT states: In adult patients intubated in ICU (P), how does daily use of Chlorohexidine (I) compared to not using (C) reduce the risk of Ventilator Acquired Pneumonia (VAP) (O) over three months? (T)
Literature Search
Because this project aims to improve nursing care and patient outcomes, I undertook a rigorous search to identify various published shreds of evidence that could help support the project change. Various sources with reputable information were searched. Such include Medline, ProQuest, Google Scholar, PubMed, Scopus, CINAHL, and Science Web. The initial step of the search involved finding the overall information about VAP. Keywords such as VAP prevention, Clorohexidine’s uses, and VAP’s effects in ICU patients were used. Besides, the use of Medical Subject Headings (MeSH) helped find evidence. Various levels of evidence, including systemic reviews, meta-analysis, quantitative, clinical trials, and qualitative publications, were identified, with sources published within the past five years meeting the inclusion criteria.
Evaluation of the Literature.
Research Questions
The various publications identified aimed at addressing various issues while answering some clinical questions. Therefore, the different objectives attracted various research questions. To begin with a study by D’Journo et al. (2018), the authors aimed to evaluate the impact of CHG on preventing complications for post-surgery patients. The question stated, Does the use of CHG prevent respiratory complications post-surgery for patients with lung cancer? In another meta-analysis by Jackson and Owens (2019), the question states, `How does the use of CHG prevent VAP among intubated patients? While mathematical analysis by Reagan et al. (2019) aimed at finding out the effectiveness of CHG in reducing the cost of care, a study by Pallotto et al. (2019) sought to find out the effectiveness of using a soap-like solution of CHG would be effective in reducing the incidences of hospital-acquired infections. Finally, Deschepper et al. (2018) stated, Does the use of chlorohexidine oral care in critical and non-critical patients reduce mortality? While Triamvisit et al. (2021) questioned whether the risk of VAP in the neurosurgical unit could be reduced by using CHG.
Sample Comparison
Every study that was evaluated had various interests; hence, diverse populations were recruited to meet the objectives of each study. The studies comprised nurses and patients admitted to the ICU. For instance, the study by D’Journo et al. (2018) and Pallotto et al. (2019) was done in different settings, but the sampled population was 450 and was randomized with a simple method. A study by Triamvisit et al. (2021) had only 291 patients despite being done in two different units. A simple randomization technique was used to divide the patients into control and intervention groups. A mathematical model by Reagan et al. (2019) used a simulated sample size of 850 to estimate the cost. Lastly, a study by Deschepper et al. (2018) used a larger sample size of 82,274 compared to the other studies.
Study Findings.
Despite various levels of evidence chosen for the literature review, all authors agreed that VAP is a serious health concern that, if not addressed, will continue being a healthcare model while increasing mortality rates. Additionally, nursing-driven care protocols are essential in improving the quality of care and health outcomes. The findings from a retrospective study by Deschepper et al. (2018) were complemented by a systematic review by Jackson and Owens (2019), as both found that the use of CHG leads to a significant reduction in HAIs such as VAP in intubated patients. Additionally, patient outcomes improved with a reduction in the hospital stay. Likewise, while assessing the role of CHG on the cost of care, Reagan et al. (2019) found that using CHG leads to a reduction in the incidences of VAP leads, a reduction in hospital stays, and a lower cost of care. Furthermore, findings from D’Journo et al. (2018) showed a significant reduction in HAIs. However, there was no significant difference in the length of stay between the control and the intervention group. Therefore, various authors recommended the implementation of CHG use in various settings to prevent various HAIs and improve patient outcomes.
Nursing Theory Utilized
This project adopted Rodger`s Change theory. As an extension of Lewin`s theory, this theory states that change is exciting and good. However, the adoption of changes is the main issue (Lingerfelt & Hutson, 2021). While Lewin`s theory appreciates the presence of resistance and forces that require the forces to push through to overcome resistance, Rodgers agrees that people may reject change but may accept it once they have seen the impact. This concept applies in nursing, especially when introducing a change that contradicts the existing norm. Individuals will always stick to what they are used to despite appreciating that the contrary is better. To implement change and make it appreciated, Rodger`s theory presents a five-step model that, if followed, can improve change adoption. The stages in their order include awareness, which involves acquiring knowledge about a new change; interest stage, which involves an individual seeking more information about an issue they have just discovered; assessment, which involves making a decision based on the accessed information either to accept or reject; execution involves accepting a change and putting it into practice, and adoption involves the continuous practice of the new idea making it a routine (Lingerfelt & Hutson, 2021). This theory is applicable to this project and allows nurses to adopt the use of CHG daily. Therefore, mastering all the stages is paramount to enabling people to adapt to change.
Implementation Plan with Outcomes
An appropriate implementation plan ensures the stepwise introduction of the change and maintaining it within an organization. This project aims to implement the use of CHG mouthwash on patients with mechanical ventilation to reduce the incidences of VAP. The initial implementation plan will identify the stakeholders who are essential in implementation. The second thing would be surveying nurses to assess their level of knowledge about the change project. This aims at identifying the gaps that would be addressed while making adjustments. Furthermore, nurses will be educated through demonstrations and presentations on how to administer CHG to help in improving knowledge and skills about the change project. Thereafter, nurses will be allowed to demonstrate the skills based on the training. Nevertheless, the expected outcome would be improved knowledge and skills for nurses on the application while adhering to the procedure daily. Another expected outcome would be a reduction in the incidences of VAP with improved clinical outcomes, reduced mortality and morbidity, and a reduction in hospital stay and cost of care. Finally, I expect the nurses to share their knowledge and skills with other healthcare personnel to enhance patient safety.
Evidenced-based Practice used in the Intervention Plan
Various levels of evidence have shown how effective CHG is in the prevention of VAP and other HAIs. Because the population of concern is intubated patients, the intervention plan aims at reducing the microbial load. Therefore, the intervention will include the application of CHG mouth daily to improve oral hygiene and kill micro-organisms. Besides, CHG wipes would be used to wipe and disinfect equipment used in mechanical ventilation.
Plan for Evaluating the Intervention
Upon implementation of the project, an evaluation will be paramount to monitor progress. Evaluation provides an opportunity for comparing the results of the pre- and post-intervention period. Data would be collected three months after implementing the change. Both qualitative and quantitative data collection methods would be used. Performing interviews with nurses to assess their experience using the intervention would form the qualitative data. Quantitative data will include structured questions with a clinical pulmonary intervention scale. A positive outcome would be marked by increased knowledge, adherence to daily bathing, and a reduction in incidences of VAP. Contrary results would mean failure, which requires adjustments to ensure that primary objectives are met.
Implementation Barriers and Measures to Overcome.
Implementation of the project requires the support of both the leadership of the organization and fellow members, failure to attain either can impair the implementation. Regarding the organization, various barriers include a lack of support from the organization, limited resources, and limited time to allow EBP changes. Because resources form a vital part of care, a lack of resources such as money and materials can impair demonstration or adherence to protocols. Besides, an inadequate resource is a trigger for nursing burnout, which can limit implementation and reduce the quality of care. Therefore, there is a need to address organizational challenges and improve the chances of success. One of the ways is through the identification of stakeholders who will mobilize the resources required for implementation. Another way is through holding genuine discussions with leadership while stressing the importance of the change project, why it should be implemented, and how it will influence clinical outcomes and patient experience. This aims to convince the leadership and enhance the implementation process.
Looking at the personal factors that impair implementation, resistance to change by members is the most common. Resistance to change can be attributed to a lack of knowledge about the change project, lack of interest, poor communication strategies, personal differences, and ignorance (Chen et al., 2022). Other personal factors include impaired teamwork, poor coordination, increased workload, limited time, and the view that a particular change will not cause maximum effects. Therefore, adopting good communication techniques will help pass the information about the project to enhance knowledge and understanding. Another strategy includes allowing for inclusivity of all members to allow them to provide their contribution, having a flexible implementation plan, solving any differences that arise, and having a resistance plan. The resistance plan allows one to appreciate other people`s different opinions while addressing them to attain understanding. Failure to identify and address the barriers on time can impair the implementation process while weakening the project.
Conclusion
Despite the presence of various driven protocols to increase patient outcomes in the ICU, various nosocomial infections, such as VAP, continue to affect ICU patients. Such conditions impair their life and increase the risk of death due to complications. The fact that most patients are immunocompromised, sedated, and with low sensorium further increases the risk of VAP, in addition to the use of mechanical ventilation. Sadly, VAP interferes with recovery and increases hospital stay by increasing the cost of care. Therefore, implementing a nurse-driven protocol such as daily bathing with CHG is essential in every setup to reduce infection rates while improving clinical outcomes. However, anticipating implementation barriers and measures to overcome them can address various barriers.
References
Chen, R., Liu, Y., Zhang, X., Yang, Q., & Wang, X. (2022). Risk factors and nursing countermeasures of ventilator-associated pneumonia in children in the intensive care unit. Journal of Healthcare Engineering, 2022, 9055587. https://doi.org/10.1155/2022/9055587
D’Journo, X. B., Falcoz, P.-E., Alifano, M., Le Rochais, J.-P., D’Annoville, T., Massard, G., Regnard, J. F., Icard, P., Marty-Ane, C., Trousse, D., Doddoli, C., Orsini, B., Edouard, S., Million, M., Lesavre, N., Loundou, A., Baumstarck, K., Peyron, F., Honoré, S., … Thomas, P. A. (2018). Oropharyngeal and nasopharyngeal decontamination with chlorhexidine gluconate in lung cancer surgery: a randomized clinical trial. Intensive Care Medicine, 44(5), 578–587. https://doi.org/10.1007/s00134-018-5156-2
Deschepper, M., Waegeman, W., Eeckloo, K., Vogelaers, D., & Blot, S. (2018). Effects of chlorhexidine gluconate oral care on hospital mortality: a hospital-wide, observational cohort study. Intensive Care Medicine, 44(7), 1017–1026. https://doi.org/10.1007/s00134-018-5171-3
Jackson, L., & Owens, M. (2019). Does oral care with chlorhexidine reduce ventilator-associated pneumonia in mechanically ventilated adults? British Journal of Nursing (Mark Allen Publishing), 28(11), 682–689. https://doi.org/10.12968/bjon.2019.28.11.682
Kohbodi, G. A., Rajasurya, V., & Noor, A. (2022). Ventilator-associated Pneumonia. https://pubmed.ncbi.nlm.nih.gov/29939533/
Lingerfelt, C. N., & Hutson, S. P. (2021). A concept analysis of dependence using Rodgers’ Evolutionary Method. Issues in Mental Health Nursing, 42(5), 451–462. https://doi.org/10.1080/01612840.2020.1820118
Pallotto, C., Fiorio, M., De Angelis, V., Ripoli, A., Franciosini, E., Quondam Girolamo, L., Volpi, F., Iorio, P., Francisci, D., Tascini, C., & Baldelli, F. (2019). Daily bathing with 4% chlorhexidine gluconate in intensive care settings: a randomized controlled trial. Clinical Microbiology and Infection: The Official Publication of the European Society of Clinical Microbiology and Infectious Diseases, 25(6), 705–710. https://doi.org/10.1016/j.cmi.2018.09.012
Pawlik, J., Tomaszek, L., Mazurek, H., & Mędrzycka-Dąbrowska, W. (2022). Risk factors and protective factors against ventilator-associated pneumonia-A single-center mixed prospective and retrospective cohort study. Journal of Personalized Medicine, 12(4), 597. https://doi.org/10.3390/jpm12040597
Reagan, K. A., Chan, D. M., Vanhoozer, G., Stevens, M. P., Doll, M., Godbout, E. J., Cooper, K., Pryor, R. J., Hemphill, R. R., & Bearman, G. (2019). You get back what you give: Decreased hospital infections with improvement in CHG bathing, mathematical modeling, and cost analysis. American Journal of Infection Control, 47(12), 1471–1473. https://doi.org/10.1016/j.ajic.2019.07.003
Suljevic, I., Asotic, D., Surkovic, I., Turan, M., & Spahovic, H. (2020). Frequency of ventilator-associated pneumonia in patients in the intensive care unit. Medical Archives (Sarajevo, Bosnia, and Herzegovina), 74(4), 285. https://doi.org/10.5455/medarh.2020.74.285-288
Triamvisit, S., Wongprasert, W., Puttima, C., Chiangmai, M. N., Thienjindakul, N., Rodkul, L., & Jetjumnong, C. (2021). Effect of a modified care bundle for prevention of ventilator-associated pneumonia in critically ill neurosurgical patients. Acute and Critical Care, 36(4), 294–299. https://doi.org/10.4266/acc.2021.00983
Xu, Y., Lai, C., Xu, G., Meng, W., Zhang, J., Hou, H., & Pi, H. (2019). Risk factors of ventilator-associated pneumonia in elderly patients receiving mechanical ventilation. Clinical Interventions in Aging, 14, 1027–1038. https://doi.org/10.2147/CIA.S197146
Professional Capstone and Practicum Reflective Journal- Topic 8 SUBMIT ASSIGNMENT
Students are required to submit weekly journal entries throughout the course. These reflective narratives help students identify important learning events that happen throughout the course and the practicum. In each week\’s entry, students should reflect on the personal knowledge and skills gained.
Write a reflection journal (250-300 words) to outline what has been discovered about your professional practice, personal strengths and weaknesses, and additional resources that could be introduced in a given situation to influence optimal outcomes. Each week there will be a specific focus to use in your reflection. Integrate leadership and inquiry into the current practice. Please make sure to address all areas in your writing.
Topic Focus: Health Policy
While APA style is not required for the body of this assignment, solid academic writing is expected.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
You are required to submit this assignment to LopesWrite. A link to the LopesWrite technical support articles is located in Class Resources if you need assistance.
Professional Capstone and Practicum Reflective Journal- Topic 9
Students are required to submit weekly journal entries throughout the course. These reflective narratives help students identify important learning events that happen throughout the course and the practicum. In each week\’s entry, students should reflect on the personal knowledge and skills gained.
Write a reflection journal (250-300 words) to outline what has been discovered about your professional practice, personal strengths and weaknesses, and additional resources that could be introduced in a given situation to influence optimal outcomes. Each week there will be a specific focus to use in your reflection. Integrate leadership and inquiry into the current practice. Please make sure to address all areas in your writing.
Topic Focus: Leadership and Economic Models
While APA style is not required for the body of this assignment, solid academic writing is expected.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
You are required to submit this assignment to LopesWrite. A link to the LopesWrite technical support articles is located in Class Resources if you need assistance.
Capstone Project Change Proposal Presentation for Faculty Review and Feedback
Create a 10-15 slide Power Point presentation of your evidence-based intervention and change proposal to be disseminated to an interprofessional audience of leaders and stakeholders. Include the intervention, evidence-based literature, objectives, resources needed, anticipated measurable outcomes, and how the intervention would be evaluated. Submit the presentation in the digital classroom for feedback from the instructor.
While APA style is not required for the body of this assignment, solid academic writing is expected, and documentation of sources should be presented using APA formatting guidelines, which can be found in the APA Style Guide, located in the Student Success Center.
Benchmark – Professional Capstone and Practicum Reflective Journal
Students are required to maintain weekly reflective narratives throughout the course to combine into one course-long reflective journal that integrates leadership and inquiry into current practice as it applies to the Professional Capstone and Practicum course.
In your journal, you will reflect on the personal knowledge and skills gained throughout this course. The journal should address a variable combination of the following, depending on your specific practice immersion clinical experiences:
New practice approaches
Intraprofessional collaboration
Health care delivery and clinical systems
Ethical considerations in health care
Population health concerns
The role of technology in improving health care outcomes
Health policy
Leadership and economic models
Health disparities
Students will outline what they have discovered about their professional practice, personal strengths and weaknesses that surfaced, additional resources and abilities that could be introduced to a given situation to influence optimal outcomes, and finally, how the student met the competencies aligned to this course.
While APA style is not required for the body of this assignment, solid academic writing is expected, and in-text citations and references should be presented using APA documentation guidelines, which can be found in the APA Style Guide, located in the Student Success Center.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
You are required to submit this assignment to LopesWrite. A link to the LopesWrite technical support articles is located in Class Resources if you need assistance.
Benchmark Information
This benchmark assignment assesses the following programmatic competencies:
RN to BSN
1.3: Understand and value the processes of critical thinking, ethical reasoning, and decision making.
2.6: Promote interprofessional collaborative communication with health care teams to provide safe and effective care.
3.2: Utilize patient care technology and information management systems.
4.2: Preserve the integrity and human dignity in the care of all patients.
5.5: Provide culturally sensitive care.